"The mind is everything. What you think, you become. What you feel, you attract. What you imagine, you create." — Buddha
In our medical practice, we’ve seen an increase in the expression of cognitive decline. Historically those who came in specifically for cognition felt they were beginning to lose their once extraordinary executive skill set. Their goal was to restore and even go beyond where they once had been.
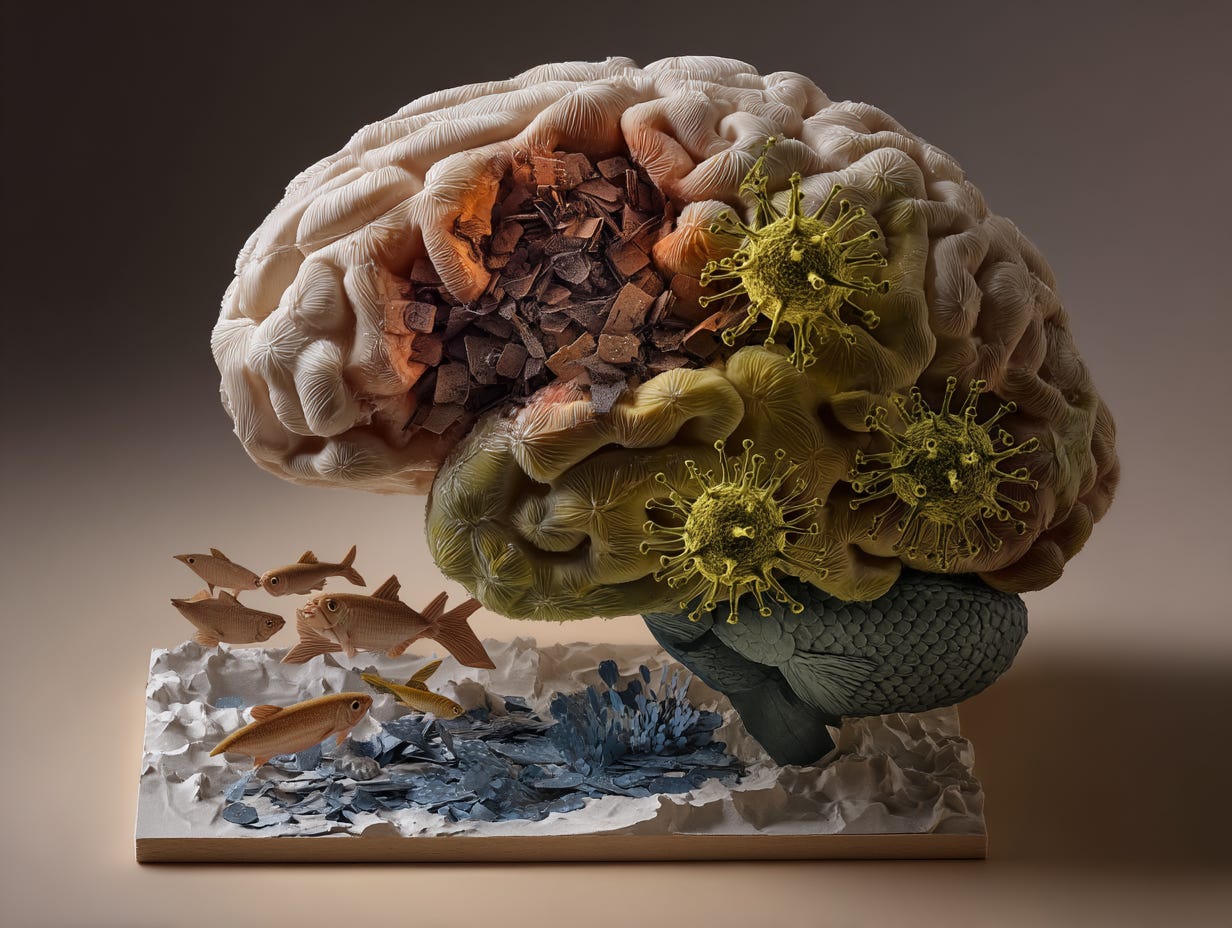
Since covid there has been more frequently reported symptoms of brain fog and the brain shutting down where it once had been able to keep going or that word finding was not as easy, memory less sharp. There is also a more consistent, active focus on ensuring they maintain sharp cognition for life. This was usually confirmed by finding a peak alpha frequency that dropped from previous levels.
The mainstream statistics are sobering: by 2050, approximately 13 million Americans aged 65+ may have Alzheimer's disease, up from 7 million in 2025. Projections indicate that over 42% of Americans aged 55+ will develop some form of dementia in their lifetime, with annual U.S. cases expected to double to 1 million by 2060.
While this sounds alarming, there is an empowering truth: this isn't simply an inevitable fate. This is an opportunity to create a new expression, one that values and demonstrates the importance of focusing on the wholeness of the complex system we are.
Recent research reveals that a significant portion of dementia cases could be prevented or potentially reversed through targeted interventions. Here I share why understanding dementia risk factors is important for extending not just your lifespan, but your healthspan.
The Multidimensional Nature of Dementia Risk
Dementia isn't a single condition but rather a collection of symptoms affecting memory, thinking, and social abilities significantly enough to interfere with daily functioning. While Alzheimer's disease accounts for 60-80% of cases, there are several types including vascular dementia, Lewy body dementia, frontotemporal dementia, and mixed dementia.
The conventional approach to dementia has long focused on isolated symptoms or genetic predisposition, yet this perspective is dangerously incomplete. For decades, many health conditions have been treated as singular, quantifiable entities measured by specific biomarkers. As our understanding evolves, it becomes increasingly clear that complex conditions like dementia emerge from the intricate interplay of physiological, cognitive, social, environmental, and even spiritual factors.
To make meaningful progress, we can shift from a fragmented, symptom-focused model to a more nuanced, systems-based approach that identifies and addresses root causes.
Metabolic Factors: The Brain-Body Connection
The metabolic foundations of dementia are far reaching. Key factors include:
Insulin resistance and glucose dysregulation - Sometimes called "type 3 diabetes"
Mitochondrial dysfunction affecting cellular energy production
Inflammation and oxidative stress damaging neural tissue
Think of your brain as an energy-hungry organ. When metabolic processes go awry, your neural networks suffer. Many clients in my practice show early signs of insulin resistance years before cognitive symptoms appear. Regular monitoring of fasting glucose, insulin, fructosamine, and HbA1c identifies these issues before they compromise brain health.
Nutritional Considerations: You Are What You Eat
Red meat consumption has been linked to cognitive decline and ever growing research has many considering positions on the ideal reccommended intake. Recent research published in 2024 found that eating just two weekly servings of processed red meat, like bacon, sausage, or hot dogs, raised dementia risk by 14% compared to people eating less than three servings per month. Each daily serving was associated with nearly two years of accelerated cognitive aging. Interestingly, swapping a serving of processed meat for nuts, beans, fish, avocado, or berries lowered dementia risk by 20%.
Micronutrient deficiencies and gut health also play crucial roles in cognitive function. The gut-brain axis, the biochemical signaling between your gastrointestinal tract and nervous system, can profoundly influence cognitive health. I will be doing an entire newsletter on this topic in the near future.
Questions for you:
How often do I consume processed meats weekly?
Am I getting adequate omega-3 fatty acids through my diet?
Have I checked my vitamin B12, vitamin D, and folate levels recently?
Infectious Factors: Hidden Triggers
Several infectious agents have been associated with increased dementia risk:
Herpes viruses - Recent large-scale studies and systematic reviews confirm that herpes simplex virus type 1 (HSV-1) - the common cause of oral herpes-is associated with a significantly increased risk of developing dementia, including Alzheimer’s disease. Learn what can be done to significantly diminish this risk in Part 3.
Lyme disease
COVID-19 - Increasingly linked to both short-term cognitive impairment and long-term dementia risk, particularly in older adults. Emerging evidence highlights multiple mechanisms connecting SARS-CoV-2 to neurodegeneration: https://www.perplexity.ai/search/there-seems-to-be-quite-a-bit-ux.bxvKcQxij6QAl3L0DVQ#13
Periodontal disease (gum infection)
This is one of the essential areas the medical establishment seems to have missed. A comprehensive health screening must include a periodontal health assessment and monitoring for chronic viral activation. There are several oral microbiome tests that I find valuable (Bristle Health). The inflammatory response to these microbes can impact brain health years before cognitive symptoms emerge.
Recent studies are finding pathogenic oral bacteria in arterial plaques and in brain tissue.
Genetic Risk Factors for Dementia
While lifestyle factors offer significant opportunities for prevention, our genetic makeup also influences dementia risk. Understanding your genetic profile can provide valuable insights into personalized prevention strategies. Let's look at some key genetic markers associated with cognitive decline.
The APOe4 Gene: The Most Well-Known Genetic Risk Factor
The Apolipoprotein E (APOe) gene comes in several variants, with APOe4 being the most significant genetic risk factor for Alzheimer's disease:
Risk impact: Carrying one copy of APOe4 increases Alzheimer's risk 2-3 fold, while two copies elevate risk 8-12 fold
Population prevalence: Approximately 25% of people carry at least one copy of APOe4
Mechanism: APOe4 affects amyloid beta clearance and increases inflammation in the brain
Important nuance: Having APOe4 doesn't guarantee you'll develop dementia—it simply increases susceptibility
An important finding from my clinical practice: APOe4 carriers often respond differently to dietary interventions. While standard dietary advice recommends limiting saturated fat, some APOe4 carriers actually show improved cognitive markers on more targeted ketogenic-style diets that address their unique metabolic needs.
Beyond APOe4: Other Genetic Markers of Concern
I was greater to discover I did not have an APOe4 expression yet as I did a deep dive it turns out, I have a combination of other variants that significantly increase my risk. While many do not want to know this, many of these genetic risks can be modified by lifestyle and supplementation.
Several other genetic variants have been associated with increased dementia risk:
TOMM40
Function: Regulates mitochondrial protein transport
Impact: Variants can affect brain energy metabolism, accelerating cognitive decline
Relationship: Often works in tandem with APOe4 to influence dementia onset timing. Also increases risk without APOe4.
Inflammatory Gene Variants
Variants in genes regulating inflammation can significantly impact neurodegeneration:
TNF-alpha (Tumor Necrosis Factor): Governs inflammatory responses, with certain variants associated with increased neuroinflammation and faster progression of cognitive symptoms
NLRP3: Variants have been significantly associated with dementia risk, particularly Alzheimer's disease (AD) and mild cognitive impairment (MCI), through mechanisms involving neuroinflammation and gene regulation.
IL-6 (Interleukin-6): Regulates inflammatory and immune reactions, with specific polymorphisms linked to heightened neuroinflammation
CRP (C-Reactive Protein): Certain variants can increase baseline inflammation levels, potentially accelerating neurodegeneration
Blood clotting gene variants: Certain variants of Protein C and Factor 5.
IntellXXDNA offers testing options that cover all of these. That is where I discovered my significant risks and have instituted mitigation.
Lifestyle Elements: Daily Choices, Lifelong Impact
Lifestyle factors profoundly affect brain health:
Sleep quality and duration represents the brain's critical cleanup mechanism
Physical activity patterns offer neuroprotective effects
Chronic stress acts as a silent accelerator of cognitive decline
Poor sleep prevents your brain from clearing harmful proteins like beta-amyloid and metabolic waste, while regular exercise increases blood flow and neurotrophic factors that support brain health. And chronic stress? It literally shrinks key memory centers in your brain over time.
Environmental Exposures: The Invisible Influence
Environmental factors can significantly impact neurological health:
Heavy metals, air pollution, and other neurotoxins
EMF exposure considerations
Household chemicals and their potential neurological impacts
I advise all my clients with cognitive concerns to assess their home and work environments for toxin exposure and air quality (see my post on assessing indoor air quality HERE). Simple changes like using HEPA air filters, choosing natural cleaning products, minimizing plastics, and filtering drinking water can reduce neurotoxic burden.
Social & Psychological Dimensions: Connection as Protection
The social and psychological aspects of cognitive health are also key:
Social isolation and loneliness profoundly impact brain health
Chronic psychological stress disrupts HPA axis regulation
Meaning, purpose, and cognitive stimulation offer protective effects
We are wired for connection. Social bonds serve as one of the most powerful regulators of stress physiology, buffering against the effects of adversity. Conversely, social isolation, relationship conflict, and community breakdown can amplify stress reactivity.
Studies have shown that people with robust social networks have significantly lower risk of cognitive decline compared to those who are isolated. This isn't just about having friends, it's about meaningful connections that provide purpose and mental stimulation.
The Bredesen Approach: Subtypes and Personalized Intervention
Dr. Dale Bredesen's groundbreaking research suggests that Alzheimer's and cognitive decline can be categorized into several subtypes, each requiring different intervention strategies:
His clinical trials have shown promising results, with a 2022 trial involving 100 patients reporting 84% showing objective cognitive improvement, including those with advanced decline. The approach targets 36+ contributors to neuroplasticity imbalance, including insulin resistance, inflammation, and nutrient deficiencies.
The key insight from Bredesen's work is that addressing modifiable factors like chronic inflammation, vascular issues, and toxin exposure can potentially impact up to 40% of dementia cases.
Identifying your specific subtype of risk or early-stage cognitive change allows for personalized intervention that addresses the unique factors driving your situation, this is personalized precision medicine. This is why comprehensive testing is so critical; it reveals your individual risk profile rather than applying a one-size-fits-all approach.
Action Items: Your Brain Protection Plan
Starting today, here are specific steps you can take to protect your cognitive health:
1. Get Baseline Testing
Comprehensive metabolic panel with insulin and inflammatory markers
Vitamin D, B12, folate, and homocysteine levels
Sleep study if you have poor sleep quality
Cognitive assessment (even if you have no symptoms) - i.e. CNS Vital Signs
2. Optimize Your Diet
Limit processed red meat to fewer than three servings monthly
Increase plant protein sources like legumes and nuts
Ensure adequate omega-3 fatty acid intake (wild-caught fish or supplements)
Focus on colorful vegetables and berries for antioxidants
3. Enhance Your Lifestyle
Prioritize 7-8 hours of quality sleep
Exercise at least 30 minutes daily (even walking counts!)
Practice stress management through meditation, breathwork, or other techniques
Create regular social engagement opportunities
4. Reduce Environmental Toxins
Test your home for mold and heavy metals
Use natural cleaning products
Install a quality water filter
Consider HEPA air filtration
5. Build Cognitive Reserve
Learn new skills (language, instrument, craft)
Engage in challenging mental activities
Maintain meaningful social connections
Practice mindfulness to improve attention
Conclusion: Prevention Is Possible
The truth is that up to 40% of dementia cases could be prevented or delayed by addressing 14 risk factors across the lifespan. The key is understanding that cognitive decline doesn't happen overnight, it develops gradually over decades, giving us multiple opportunities for intervention.
I've witnessed remarkable improvements in clients who implement comprehensive preventive strategies early. Even those with mild cognitive impairment often see significant stabilization or improvement when addressing the multidimensional factors we've discussed. I believe that these interventions will slow progression or reverse it in most of this population.
The rising tide of dementia is real. By understanding your personal risk profile and implementing targeted interventions, you can significantly reduce your risk and protect your most precious asset - your mind.
In Part 2 of this series, I'll dive deep into specific biomarkers to monitor. In Part 3, I will outline the most effective prevention strategies based on your personal risk factors. Until then, remember that small, consistent steps toward brain health today can have profound effects on your cognitive future.
References:
Fang M, et al. Lifetime risk and projected burden of dementia. Nature Medicine. 2025 Jan 13. doi: 10.1038/s41591-024-03340-9.
Quan, M., Wang, X., Gong, M., Wang, Q., Li, Y., & Jia, J. (2023). Post-COVID cognitive dysfunction: Current status and research recommendations for high-risk population. The Lancet Regional Health – Western Pacific, 38, 100836.
Araya K, Watson R, Khanipov K, Golovko G, Taglialatela G. Increased risk of dementia associated with herpes simplex virus infections: Evidence from a retrospective cohort study using U.S. electronic health records. J Alzheimers Dis. 2025 Mar;104(2):393-402.
Kulkarni MS, Miller BC, Mahani M, Mhaskar R, Tsalatsanis A, Jain S, Yadav H. Poor Oral Health Linked with Higher Risk of Alzheimer's Disease. Brain Sci. 2023 Nov 7;13(11):1555.
Eke PI, Thornton-Evans GO, Wei L, Borgnakke WS, Dye BA, Genco RJ. Periodontitis in US Adults: National Health and Nutrition Examination Survey 2009-2014. J Am Dent Assoc. 2018 Jul;149(7):576-588.e6.
Inga Prokopenko, Gentaro Miyakawa, Bang Zheng, Jani Heikkinen, Daniela Petrova Quayle, Chinedu Udeh-Momoh, Annique Claringbould, Juliane Neumann, Hazal Haytural, Marika A. Kaakinen, Elena Loizidou, Esther Meissner, Lars Bertram, Djordje O. Gveric, Steve M. Gentleman, Johannes Attems, Robert Perneczky, Thomas Arzberger, Pierandrea Muglia, Christina M. Lill, Laura Parkkinen, Lefkos T. Middleton, Alzheimer's disease pathology explains association between dementia with Lewy bodies and APOE-ε4/TOMM40 long poly-T repeat allele variants, Alzheimer's & Dementia: Translational Research & Clinical Interventions, Volume 5, 2019, Pages 814-824,












Thank you, Dr. Stickler, for shining a spotlight on what Alzheimer’s Disease International calls a looming “tsunami” —dementia cases are projected to almost triple to 139 million by 2050 if we do nothing. Early action matters because many of the first clues are easy to wave away: irritability, momentary word-finding pauses, or quiet withdrawal from hobbies can all precede obvious memory loss.
The hopeful news is that as much as 40-45 percent of dementia risk is tied to modifiable lifestyle factors — nutrition, movement, restorative sleep, stress regulation, and rich social connection all help build the “cognitive reserve” that buffers the aging brain. Your call for proactive screening dovetails with the newest clinical guidance from neurologists, who now emphasize blood-pressure control, aerobic exercise, and anxiety reduction as front-line brain-sparing tools long before disease shows up on a PET scan.
In other words, every walk around the block, every leafy-green meal, every deep conversation is a small deposit into our neural savings account. The sooner individuals, communities, and healthcare systems align around this prevention-first mindset, the more resilient our collective future becomes. Grateful for the clarity and urgency you bring to the conversation — here’s to an infinity of daily choices that protect the mind of humanity.
It's very important to understand the role of glutathione and detoxification . Dr Alan Pressman suggested to improve the supply of the building blocks of glutathione. The tripeptide is made up of cysteine,glycine,and glutamate acid . It is also important that methylation process is functioning well. It has been noted that the over consumption of simple sugars sets up a condition of glycation where you are burning yourself up from the inside. The micronutrients that are essential for metabolic processes to function properly mostly come from leafy greens and the rainbow of fruits and vegetables. Of course a supply of clean water is essential to keep the detoxification process running smoothly. Getting up and moving around improves your chances of detoxification . Think of fiber and water as a power wash to broom out metabolic waste.
People want a medicine or a combination of nutrients to do the work for them. I don't think it's that simple the major pharmaceutical companies would like to have product to sell that would do that for you. So far there's nothing they can Market. In the meantime do the modalities that promote liver function and to keep the bionome as full of good bacteria as possible. It's been suggested that Bad bacteria in cured meats
disrupts the balance. consuming a lot of white flour glunks up the system too and interferes with Transit time. Too much alcohol causes disbiosis. That's why I called Donald Trump the disbiotic despot. I could help him feel better within a month and maybe he would be less angry the Chinese herbalists say the more toxic your liver is the more anger you have